Four Essentials You Need to Know About EMS Capnography
This article was taken from the August 2, 2021 post on RT Magazine and was written by RT Magazine Associate Editor Lisa Spear. Note: This is not an RT Magazine endorsement of MED Alliance products.
Capnography is an essential monitoring technique for cardiac patients requiring resuscitation and respiratory support. Here are four things to remember when monitoring EtCO2 in prehospital settings.
With every exhalation, the lungs emit the colorless gas carbon dioxide (CO2). Fluctuations in this waste product of the human body can provide important insights into respiratory health, disease, and can even help providers understand how patients are responding to treatments or if the patients’ conditions are improving. The most commonly used method to monitor CO2, a capnography monitor, is a mainstay in emergency medicine. These monitors are regularly used to better understand the status of patients in respiratory distress, cardiac arrest, and shock. The data gathered from these monitors can also help guide clinicians when they are intubating a patient, which is one of many of capnography’s critical functions, explains emergency medicine physician Christopher Kahn, MD, MPH, who is the chief of the Division of Emergency Medical Services and Disaster Medicine at UC San Diego Health.
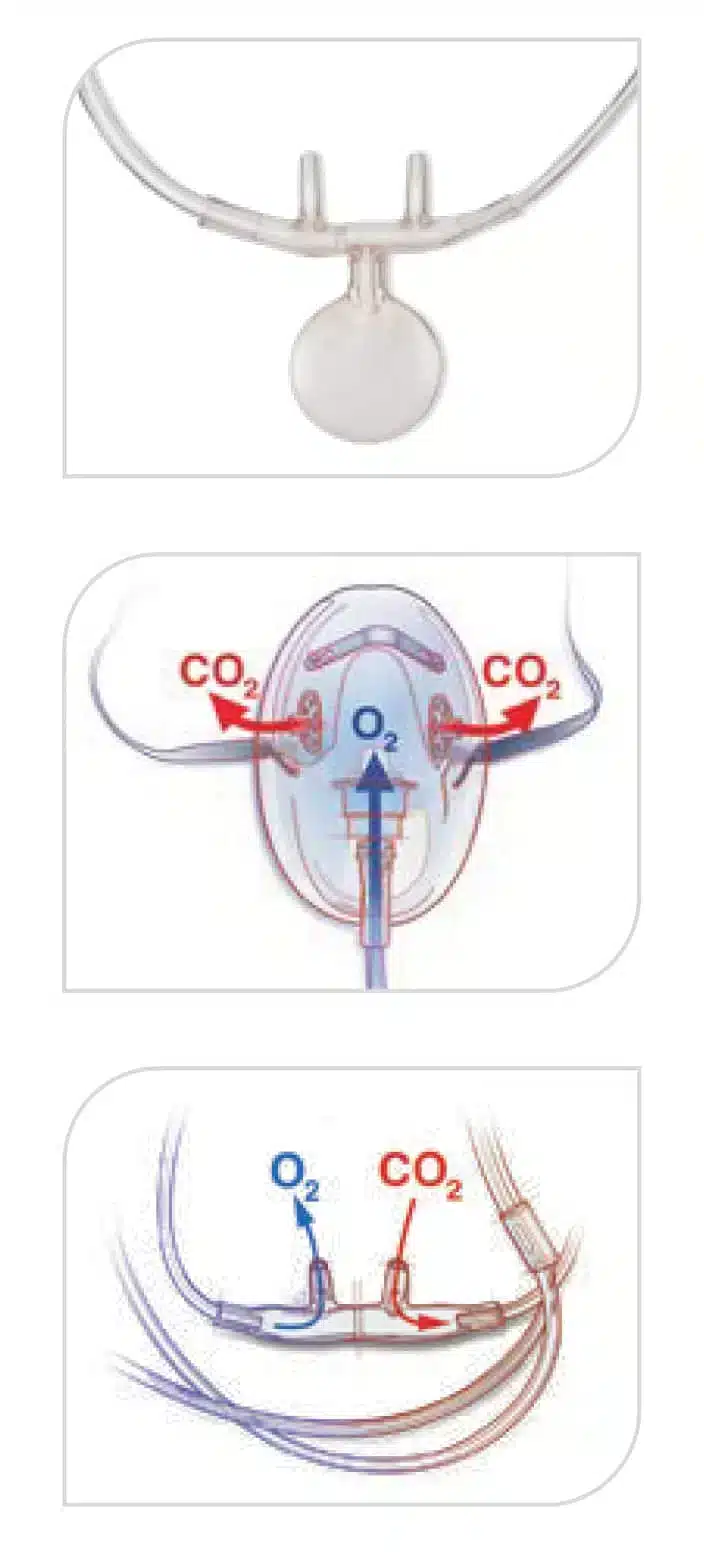
When using capnography monitors, CO2 data is captured by a sensor. Either nasal prongs can be used to capture exhaled air from patients who are breathing or those who need assisted ventilation can use an adapter that is attached to a bag valve mask and advanced airway device.
On the monitor, a number and graph will represent the amount of CO2 in exhaled air. A waveform called the capnograph will display how much CO2 is present at each stage of the respiratory cycle, which normally has a rectangular shape.
The number represents the partial pressure of CO2 that is normally found following an exhalation. This shows the end-tidal CO2 (EtCO2) reading, which in healthy people is around 35-45 mm Hg, according to information from medical device company Medtronic.
Here are four things you should know about capnography and how it can help you provide better care in prehospital settings:
1. The Importance of Capnography During Intubation
Intubation is a honed skill and clinicians can lean on capnography data to ensure that the endotracheal tube is placed correctly. “The principle behind this is that the esophagus has no carbon dioxide, but obviously the lungs have a lot of carbon dioxide,” said Baruch Krauss, MD, EdM, senior associate physician in medicine in the Division of Emergency Medicine of Boston Children’s Hospital. “So if you want to figure out if you put the tube in the right place: in the trachea as opposed to the esophagus, then you check the CO2 levels. If there is no CO2, then you probably put it in the stomach, if there is CO2, then it is in the lung,” said Krauss, an associate professor in pediatrics and emergency medicine at Harvard Medical School.
When intubating a patient, a capnography monitor shows the actual value of CO2. This differs from basic qualitative colorimetric CO2 detectors, which may only show the presence or absence of CO2, leaving clinicians with less information. If only using a qualitative colorimetric CO2 detector, which attaches to the endotracheal tube, providers may miss critical information about tube placement. For instance, if CO2 levels decrease drastically after intubation, then the tube may be placed incorrectly.
“It is not just the presence or absence of end-tidal carbon dioxide that you can get with a qualitative colorimetric device, but if we’re looking to see that the actual value is about the same, then that’s a pretty good indication that your tube is right where it needs to be. Whereas, if your numbers cut in half, the tube maybe too deep,” said Kahn. “When incubating patients, we have discovered that it is incredibly useful to have capnography in place both before and after intubation because it helps you make sure that the tubes are in the right place.”
SalterSTAT Capnography
SalterSTAT sets the standard in capnography sampling lines. The innovative designs can be used everywhere capnography is indicated, including options for reflective connector systems, mask applications and luer-style connector systems. Each provides effective CO2 detection and O2 delivery.
2. Don’t Forget to Watch the Patient
When there is a capnography monitor with a screen, it is tempting to focus on what the numbers and waveforms are communicating about the patient’s condition, but don’t let the screen distract you from the patient. “Really, the key thing in EMS is to pay attention to the patient,” explains Kahn, who is an associate professor of emergency medicine at UC San Diego in California. “As clinicians in all fields, we often find ourselves going ‘Oh hey, what does the monitor show, but it is not all about waveforms and numbers on a screen. It’s really about what’s happening with the person in front of you.”
Key things to notice include: the patient’s coloration, respiratory effort, and the sound of their breathing. Typically, in patients with a healthy respiratory system, the brain reacts to fluctuations in CO2 in the bloodstream to modulate ventilation. Clinicians assess this by watching the movement of the chest, looking for respiratory effort, counting respiratory rate, and listening to the breath.
3. Getting to The Source of Respiratory Distress
It isn’t always easy to diagnose the source of respiratory distress and treating the wrong condition may lead to further harm. Several conditions can create shallow breathing, wheezing, and crackles. Adding waveform capnography to history and physical exam findings may assist with the diagnostic process.
The shape of the capnography waveform, as well as the end-tidal number, are important indicators to differentiate between different disease states. A normal waveform is a crisp, rectangular shape, but when a patient is experiencing bronchospasm, air becomes trapped in the alveoli and is not released consistently. In these cases, the capnography waveform on the screen may appear to curve like a shark fin, with a sharp “peak,” according to information from Medtronic.
The curve may become more pronounced if the bronchoconstriction is severe. This also corresponds with higher end-tidal CO2. If the waveform is upright without the shark fin curve, there is no bronchospasm and the respiratory issue must be due to another cause. For example, in pulmonary edema cases CO2 diffuses across fluid in the lungs, and the capnography waveform will appear as a normal rectangular shape, even if the person is showing signs of respiratory distress.
4. Incorporate Capnography into Continuing Education
“Ongoing training is definitely helpful. No matter how amazing a tool you have, if it is not something that you use regularly or study with regularly then when you actually need it, you are going to be rusty with it,” said Kahn. “It is something that I would incorporate into regularly scheduled continuing education.”
Many EMS systems will have ongoing training available, which may include simulations and have clinicians actually run through the different scenarios. While it may not be feasible for some institutions to have an actual capnography monitor available during training simulations, Kahn suggests using props and visual aids.
“You can at least show a picture of a waveform and a number and have those aids visible,” said Kahn.
Clinicians can also take the initiative to include capnography into their response to training simulations. For instance, Kahn said, during a simulation a the trainers might say, “‘Here is a patient who is unconscious and not breathing on the ground, what do you do?’”
“And whether it is on a fancy medical simulator or a piece of paper on the ground that said unconscious patient, you walk your way through it and tell the instructor what it is you are doing – making sure that you incorporate end-tidal capnography into those simulations.”
For more information about SalterSTAT Capnography, call 888-891-1200 or email us to be connected to a local representative.
MED Alliance Group is a medical device distributor with more than 350 years of combined medical device sales and distribution experience. Dedicated to meeting the needs of its clinical customers and manufacturing partners, MED Alliance offers cost-effective, customized sales, logistics, and distribution solutions for products found in anesthesia/respiratory, blood/transfusion therapy, EMS/emergency room, interventional radiology/cath lab, iv/vascular and NICU/PICU.
Please follow us on LinkedIn, Facebook and Twitter for MED Alliance product updates.